Menopause has long been treated as a quiet, private ordeal. That silence carries a cost. On World Menopause Day, bringing menopause out of the shadows is not a niche concern but a public priority with tangible dividends for health, equity, and economic growth. The conversation must move from scattered efforts to a coordinated plan that is practical to implement in clinics, workplaces, and national policies.
Perimenopause and menopause can span more than a decade. At any given moment, more than 450 million women worldwide are navigating this transition. According to research by the World Economic Forum’s Global Alliance for Women’s Health, closing the women’s health gap on menopause alone could yield an estimated 2.4 million disability adjusted life years every year and roughly 120 billion dollars in annual GDP gains. These figures represent fewer missed workdays, steadier household income, and less strain on health systems. They also represent lives experienced with more comfort, clarity, and confidence. Numbers summarize the stakes, but lived experience explains them.
What stands in the way is not a lack of need but a lack of preparation across the systems that touch women’s lives. Diagnosis and care are often late, inconsistent, or inaccessible. And there is evidence to back this — a Yale University review of insurance claims showed while 60% of women with significant symptoms of menopause seek treatment, almost 75% are left untreated. Training is part of the problem. In one study, half of family medicine doctors reported only a single lecture on menopause during training, and one in five reported none at all. The workforce impact is visible. Research indicates that one in four women has considered leaving work during the transition, and one in ten who have worked through menopause left a job because of their symptoms. This is not only a productivity story, it is also one of opportunity cost. It is a story about experienced leaders stepping back, about teams losing anchors, and about families absorbing avoidable stress.
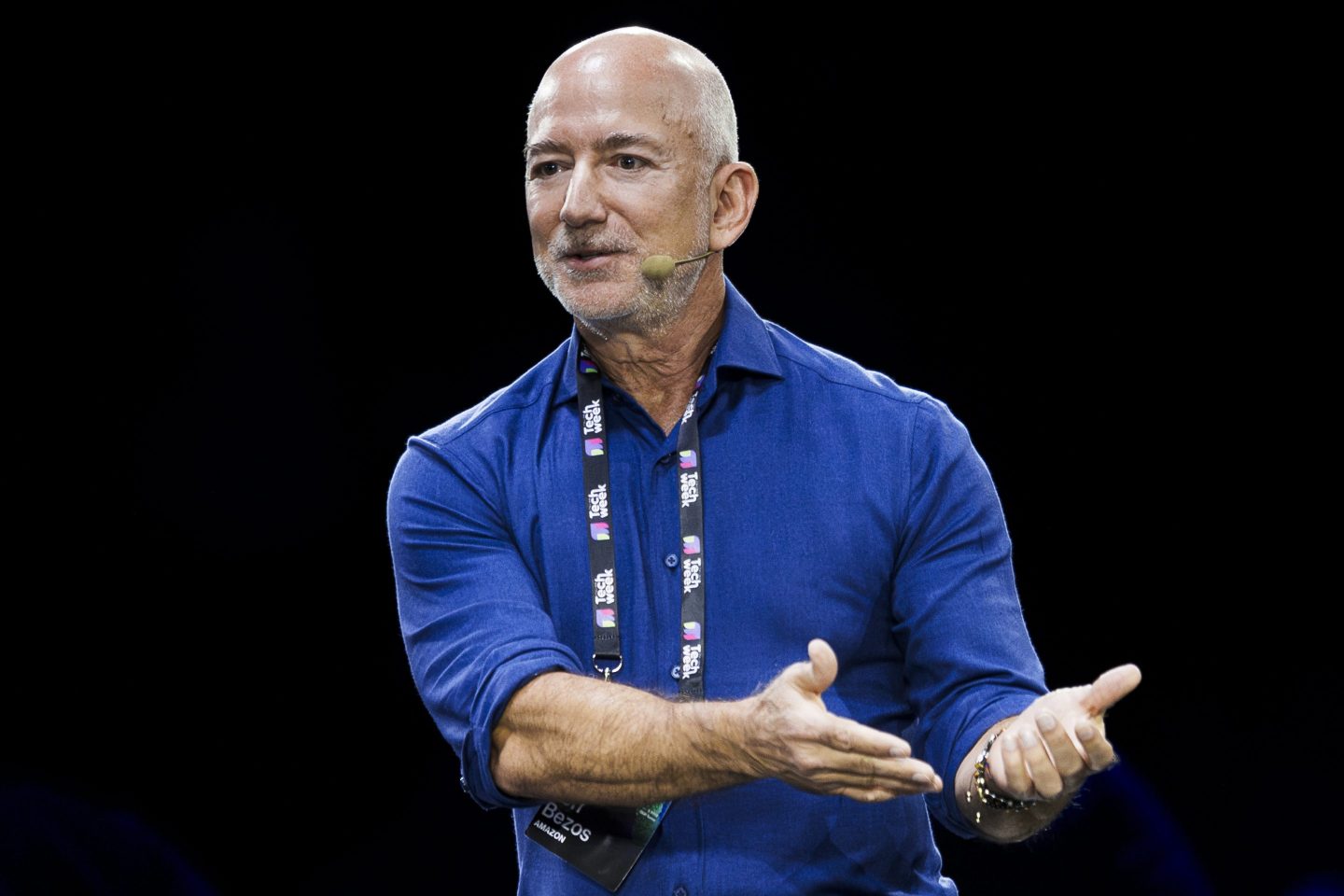
As an Expert Member of the one-of-its-kind multistakeholder platform, the World Economic Forum’s Global Alliance for Women’s Health, as well as an expert medical advisor at acclaimed actress, director, producer, advocate, and entrepreneur, Halle Berry’s menopause care platform, Respin Health, I see how quickly the conversation shifts when evidence meets execution. These organisations are helping translate science into clinical standards and employer policies, while informing policy frameworks that leaders can adopt and fund. Advocacy is meaningful when it results in actions that are easy to copy, measure, and sustain. Our work with Halle Berry, who recently joined the Global Alliance for Women’s Health as Public Ambassador, showcases the sheer appetite and momentum that exists to redefine menopause and empower women to be the guardians of their own health. The path is known. What remains is follow-through.
“When we leave women to figure menopause out alone, we pay a grave price in health, productivity, and our very own dignity. We have to normalize this conversation about menopause. We have to make guidance useable. We have to improve access to quality care, and we need to invest in research and innovation,” said Halle Berry.
Health care is the first place to start
Menopause should be part of routine primary care, not a specialty service that only a few can reach. Screening can begin during routine visits for women in their forties and fifties, with clear pathways for counselling and treatment. Evidence based options include lifestyle approaches, non-hormonal treatments, and, when appropriate and safe, hormonal therapies guided by informed choice. Care should consider mental health and cardiometabolic risk, since sleep disruption, mood changes, and metabolic shifts often travel together. Referral pathways must connect primary care, gynaecology, mental health, and cardiometabolic services so women are not left to navigate a maze with contradictory advice. This is not about boutique clinics for the few. It is about equipping the front lines to meet a ubiquitous need.
Workplaces are the next lever. Simple adjustments can make a meaningful difference. Flexibility where feasible, paid time off for symptom flare days, and practical measures like temperature control and quiet rest areas reduce the friction that turns symptoms into lost days. Benefits should name menopause explicitly, so women know coverage exists. Manager training should normalize support without forcing disclosure. Employers who measure retention, error rates, and team performance before and after adopting these practices will find what many have already learned. Small investments stabilize teams and pay for themselves.
Research and product design must close the data gap and raise the bar for solutions. Studies should reflect the diversity of real women, including race, age, and co existing conditions. Endpoints should be comparable so clinicians and consumers can tell what works and for whom. Digital tools and consumer products that target sleep, cognition, thermoregulation, and pelvic health should be evaluated against evidence standards and priced for broad access. Innovation is welcome. So is rigor. Women deserve both.
Policy and financing can turn best practice into the baseline
Essential menopause services belong in national primary health packages and in public and private insurance coverage. Governments can accelerate employer adoption with clear standards, public recognition, and targeted incentives that reward organizations for implementing menopause supportive policies. Public information campaigns can replace stigma with practical knowledge for women, partners, managers, and clinicians. Countries should publish a small set of indicators that matter in daily life. Time to diagnosis, treatment access, and workforce participation are simple to understand and powerful to track. Accountability is easier when the yardstick is clear.
Why does this matter beyond the clinic and the workplace? Because when women’s health is prioritized, families and economies function better. Earlier diagnosis and appropriate treatment reduce absenteeism. Menopause supportive workplaces keep experienced talent on the job and reduce turnover. Good care prevents avoidable complications that are costly later. These mechanisms repeat across millions of women and thousands of organizations. The cumulative effect shows up in national productivity. The more important return, however, is human. Better sleep, clearer thinking, steadier mood, and restored confidence change how women experience midlife. That is growth measured in dignity and opportunity.
Effective advocacy pairs public leadership with technical depth and coordinated action. Public figures help make the issue relatable. Researchers and clinicians define what quality care looks like. Cross-sector forums align employers, health systems, and governments on practical standards and timelines. This combination turns awareness into accountable implementation. This is where platforms such as the Global Alliance for Women’s Health and the International Menopause Society bring real value to the conversation — by bringing together experts and leaders to make the shift from intention to implementation.
What should happen now?
Health systems can add a brief screening and counselling step to routine primary care visits and build simple referral pathways that do not collapse under real world pressure. Medical schools and continuing education providers can strengthen training, so the next generation of clinicians starts on firmer ground. Employers can publish a menopause policy, train managers, and update benefits language so support is easy to find. Researchers can design studies that reflect the diversity of women and use shared endpoints that allow transparent comparisons. Policymakers can put menopause care in the basic benefit package and require transparent reporting on access and outcomes. None of these actions is a moonshot. Each is a choice that aligns with what we already know.
Culture change travels alongside policy change. Partners can listen without judgment. Friends can share what has helped them. Community leaders can include menopause in health talks that already reach women where they live and work. The tone matters. Precision matters. A plan matters. Together they create an environment where a woman does not have to spend years searching for a name for her symptoms or for a path to relief.
World Menopause Day should not be a once-a-year reminder. It should be a yearly accountability moment that asks a simple question: Did we make it easier this year for women to find accurate information, timely care, and practical support? If the answer is yes, the benefits will be visible in clinics, workplaces, homes, and countries.
The path is clear — what remains is resolve. Let us act today so more women can live, work, and thrive tomorrow.
The opinions expressed in Coins2Day.com commentary pieces are solely the views of their authors and do not necessarily reflect the opinions and beliefs of Coins2Day .