President Donald Trump has announced a landmark deal aiming to expand Medicare coverage to include certain weight-loss medications, a move that could dramatically change access to these treatments for millions of older Americans. On November 6, Trump revealed that his administration had struck agreements with Eli Lilly and Novo Nordisk, the makers of popular weight-loss drugs including Ozempic and Wegovy, to reduce costs and allow for broader Medicare coverage starting in 2026.
Under the arrangement, prices for GLP-1 drugs—used both for diabetes and obesity—will be slashed for Medicare and Medicaid beneficiaries. The prices of Ozempic and Wegovy will fall from $1,000 and $1,350 per month, respectively, to $350 when purchased through through the TrumpRx.gov website set to launch in January 2026, according to the White House’s official communication. Other products, including upcoming pills, will be available for as little as $145 per month through Medicare and Medicaid, according to a background press briefing reported by CNBC.
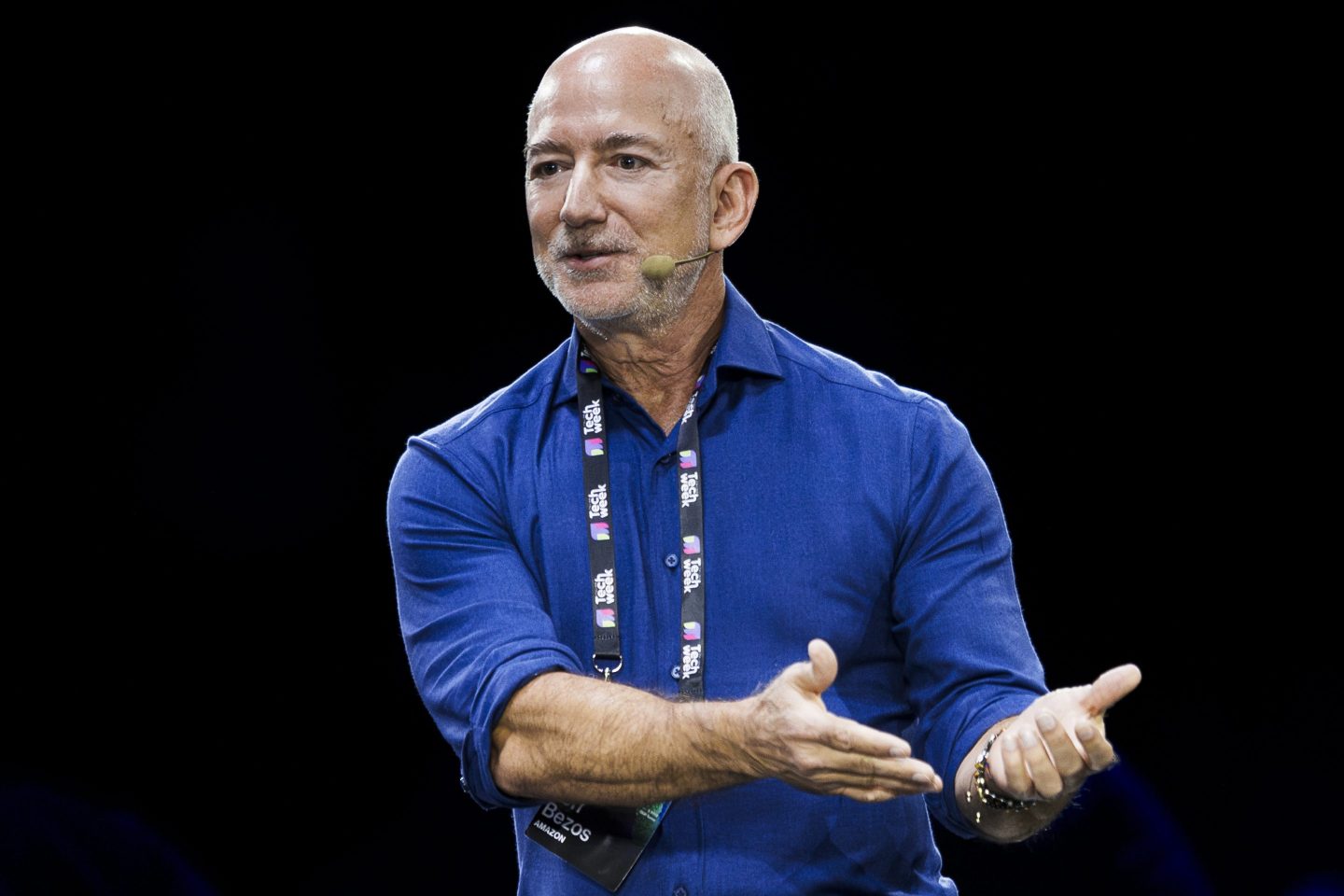
“We’re going to be paying, instead of $1,300, you’ll be paying about $150,” Trump said in mid-October while highlighting a separate drug price deal. At the time, Centers for Medicare and Medicaid Services administrator Mehmet Oz clarified that that negotiations were still ongoing.
Current Restrictions and Changing Policies
Until now, Medicare had been prohibited by law from covering medications prescribed specifically for weight reduction, a policy rooted in the 2003 Medicare Modernization Act, as noted by health news service KFF. Recent FDA approvals of new uses for drugs like Wegovy, especially for reducing the risk of heart attacks and strokes in overweight individuals with cardiovascular disease, have started to open the door for broader Medicare coverage. The Centers for Medicare & Medicaid Services (CMS) recently signaled that Part D plans can now add some of these drugs to their formularies, provided they have a medically accepted use that isn’t specifically excluded.
Despite these changes, actual Medicare coverage for weight loss alone—as opposed to additional conditions like diabetes or heart disease—has lagged behind, mainly due to longstanding federal restrictions and concerns over potential costs to the system.
Costs and Fiscal Concerns
The fiscal implications of the new coverage policy are significant. The Congressional Budget Office (CBO) has estimated that covering these anti-obesity drugs through Medicare could increase federal spending by at least $35 billion from 2026 through 2034, with average costs per user around $5,600 in 2026, though competition and negotiations could drive these numbers lower over time. The national debt topped $38 trillion just weeks ago, with budget watchdogs at the Committee for a Responsible Federal Budget and the Peter G. Petersen Foundation decrying the runaway, escalating nature of America’s insolvency.
Obesity affects about 40% of U.S. Adults, according to the Centers for Disease Control and Prevention (CDC), and nearly 39% of Americans age 60 and older are affected, although obesity rates have started falling in many states for the first time in a decade, likely due to weight-loss medication’s impact.